Few scientific stories are told as often—and as dramatically—as the tale of a messy benchtop and a Petri dish left out over a late-summer holiday. But the story of Alexander Fleming is more than a single eureka. It is the chronicle of a careful observer who could turn clutter into clarity, and chance into change. Long before penicillin altered the arc of 20th-century health, the habits that define the Alexander Fleming biography were already in place: keep good notes, doubt easy explanations, and ask better questions when results look “wrong.”
Read as a working biography rather than legend, the Alexander Fleming biography becomes a guide to scientific attention. The Scottish farm boy who learned patience from weather became a London bacteriologist who trusted what he saw with his own eyes more than he trusted fashion or habit. And when nature drew a neat, bacteria-free halo around a drifting mold, he did not throw the plate out; he asked a better question. That stance—observe, test, revise, collaborate—turns a laboratory accident into a civic advance.
Alexander Fleming biography: Early Life, Training, and the Making of an Observer
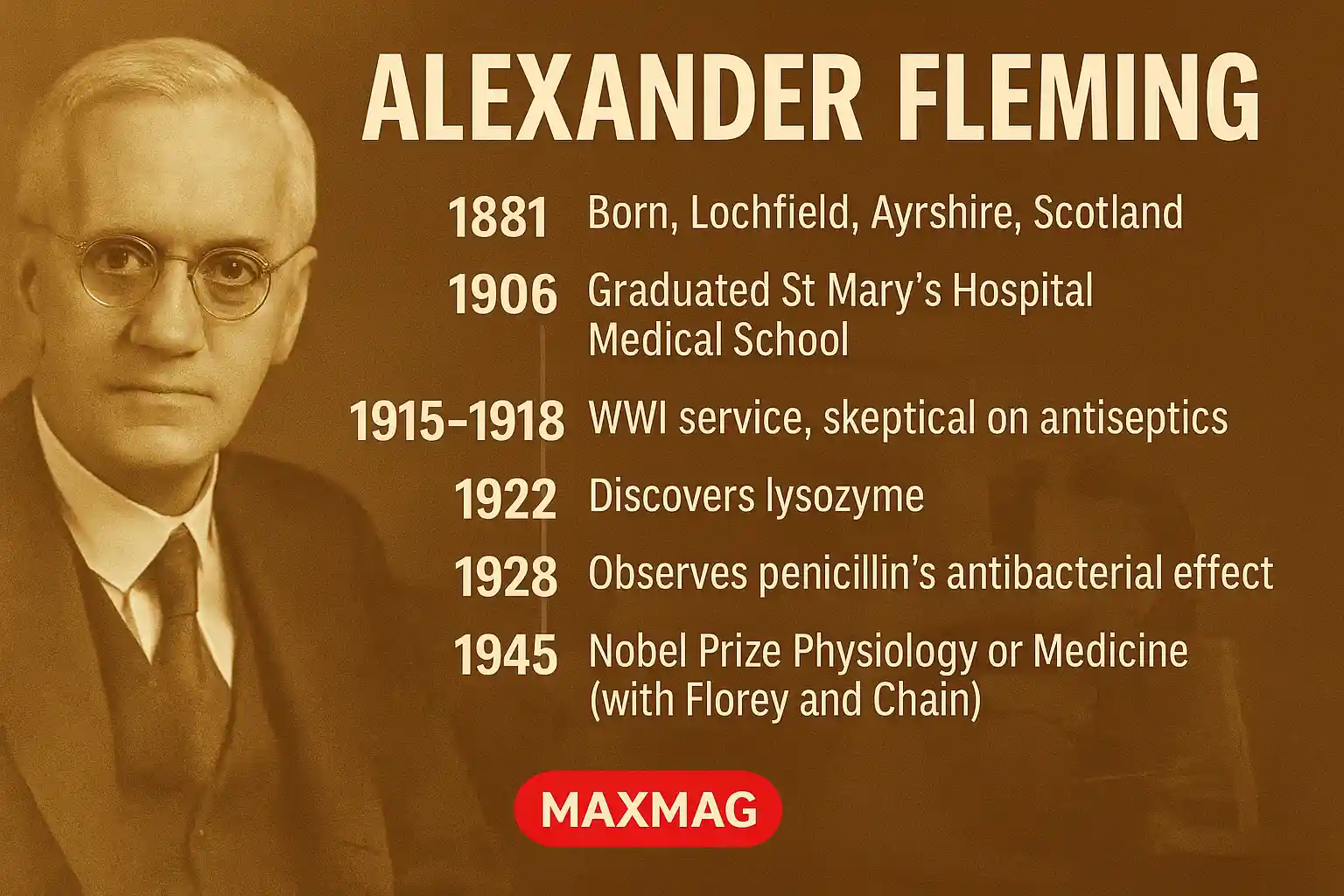
Born in 1881 on a farm at Lochfield, near Darvel in Ayrshire, Scotland, Fleming grew up where thrift and watchfulness were not virtues so much as necessities. Those disciplines shaped the Alexander Fleming biography before laboratories did. As a young man in London, he joined St Mary’s Hospital Medical School, soon gravitating to bacteriology under the charismatic Sir Almroth Wright. The apprenticeship mattered: it turned an agile medical student into a clinician-scientist who prized method over myth.
The First World War sharpened his skepticism. Serving in the Royal Army Medical Corps, Fleming saw wounds worsened by the very antiseptics meant to protect them. He argued that strong chemical antiseptics could injure tissues and reduce the body’s defenses—inviting the microbes they were supposed to repel. The Alexander Fleming biography therefore begins with a contrarian but humane insight: judge success by the patient’s outcome, not by the sting of an antiseptic or the neatness of a textbook protocol.
Years before the mold arrived, Fleming had already demonstrated the pattern that would define his career: notice, test, and publish with restraint. In 1922 he isolated lysozyme after observing how tears and nasal mucus could dissolve certain bacterial colonies. It was not a mass-market medicine, but it was a conceptual breakthrough—nature’s own quiet defense—foreshadowing penicillin and training a generation of eyes to look for antimicrobial clues in bodies as well as in bottles.
Alexander Fleming biography: A Petri Dish, a Mold, and a Clear Zone on the Plate
In September 1928, returning to his lab at St Mary’s after vacation, Fleming noticed an oddity on a neglected streak plate of staphylococci: a contaminating mold had landed, grown, and carved a transparent moat free of bacteria. Where others might have seen a ruined plate, he saw a conversation—one organism suppressing another. The mold was identified as a species of Penicillium, and the substance it exuded he called “penicillin.” With that observation, the Alexander Fleming biography moved from careful watching to disciplined hypothesis.
He went to work: testing heat and pH stability; comparing effects across pathogens; attempting (with limited resources) to stabilize and purify the active principle. Penicillin crushed staphylococci and streptococci, but its crude extracts degraded stubbornly. He documented what the plate showed and stopped short of claims the extract could not yet support. The measured tone—so characteristic of the Alexander Fleming biography—kept the finding credible even as others doubted its practicality.
Alexander Fleming biography — Myths, Accidents, and the Discipline of Serendipity
“Accident” hovers over the tale, but serendipity is not a method. Serendipity favors people who label plates, keep orderly benches, and look twice before cleaning up. Fleming did not create the mold; he created the conditions in which its message could be read—and he had the habits to hear it. Another myth is that he single-handedly delivered a finished drug. In truth, the Alexander Fleming biography shares its spine with the Oxford story: observation begets hypothesis; collaboration turns it into care.
Alexander Fleming biography: Oxford, Industry, and the Making of a Medicine
In the late 1930s and early 1940s, the Oxford team—Howard Florey, Ernst Boris Chain, Norman Heatley, and colleagues—returned to Fleming’s neglected lead. They purified fractions, tested them in mice, and then in desperately ill patients. The results were dramatic—fevers fell, bloodstreams cleared, wounds closed. Supply was so scarce that clinicians famously recovered the drug from patients’ urine to reuse it. At that hinge in the Alexander Fleming biography, the story crossed the Atlantic as U.S. engineers and fermentation experts joined the push to scale production.
Peoria’s deep-tank fermentation, corn-steep liquor, and a lucky high-producing strain found on a cantaloupe multiplied yields. Process science transformed a fragile lab extract into a factory product. By D-Day in 1944, penicillin was widely available, reshaping surgical and battlefield outcomes. In 1945, the Nobel Prize in Physiology or Medicine recognized Fleming, Florey, and Chain—an institutional acknowledgement that the Alexander Fleming biography is a networked achievement, not a solitary miracle.
Alexander Fleming biography in the Context of Resistance and Stewardship
Fleming warned early—and clearly—that misuse would breed resistant microbes. In his Nobel lecture he cautioned that underdosing could “educate” bacteria rather than eliminate them. Modern stewardship programs put that warning into policy: use antibiotics when indicated, at the right dose, for the right duration; narrow the spectrum when cultures return. For an authoritative public-health overview, see the CDC overview of antibiotic use and resistance. That resource and the U.S. National Library of Medicine’s MedlinePlus guide to antibiotics show how the Alexander Fleming biography still shapes frontline decisions.
Stewardship is the institutional descendant of one investigator’s laboratory manners. The logic is the same as in the Alexander Fleming biography: measure twice, act once; look for unintended effects; adjust when evidence asks you to. On hospital wards this becomes susceptibility panels, shorter effective courses, and “start smart, then focus.” In communities it means avoiding reflexive prescriptions for viral illnesses and teaching patients why finishing a course matters.
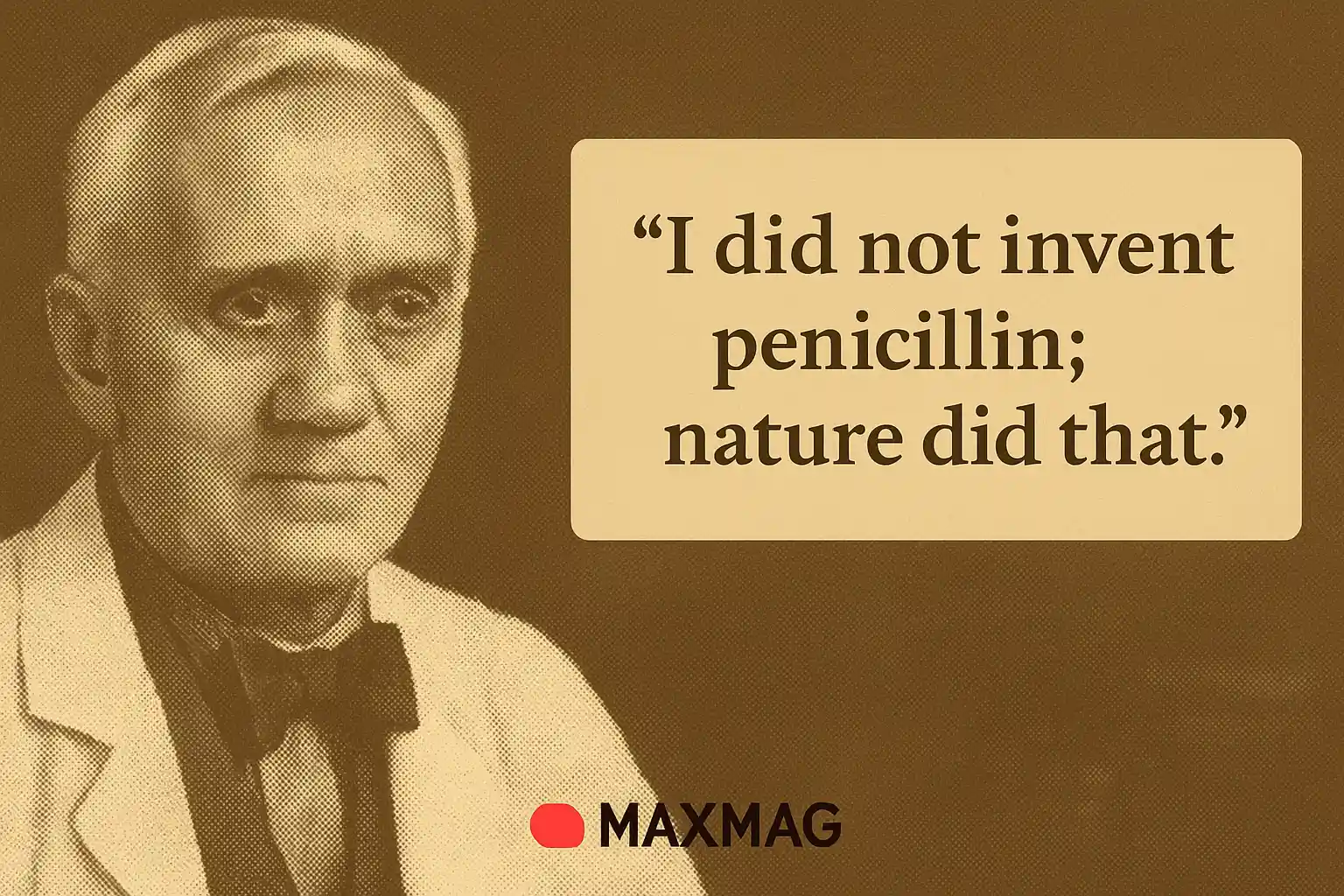
Plain Words, Lasting Warnings: Alexander Fleming in His Own Voice
(Enhanced) Fleming’s public remarks were spare, unfussy, and practical—designed less to dazzle than to nudge. He used a handful of lines to rebalance credit (“nature did that”), to reset expectations (“cures, but does not teach”), and to plant an early flag for stewardship (“do not underdose”). That economy of language is why the lines endure: each is an operating instruction for science and medicine. To anchor those lessons in the historical record, here are several compact quotations often attributed to him, followed by a sentence of context to show why they still matter.
- “I did not invent penicillin; nature did that.” — A quiet insistence that discovery begins with humility toward the living world.
- “Penicillin cures, but it does not teach.” — A reminder that a powerful drug cannot replace judgment, hygiene, and public-health practice.
- “One sometimes finds what one is not looking for.” — An ode to disciplined serendipity: prepare the stage so surprises can be seen and believed.
- “If you use penicillin, use enough.” — Practical dosing advice distilled to a maxim; underdosing invites relapse and resistance.
- “The uneducated man may easily under-dose himself and, by exposing his microbes to non-lethal quantities of the drug, make them resistant.” — An early, plain-spoken blueprint for antibiotic stewardship.
Methods and Materials: How the Work Actually Looked
Popular retellings compress the laboratory steps into a cinematic glance. In reality, the work involved repeated streaks, control plates, and tedious attempts to concentrate an active principle from broths that seemed to lose potency with every manipulation. Fleming’s notebooks show iterative changes in temperature, media, and timing; his correspondence shows the hunt for supplies and the search for colleagues who could stabilize the extract. That texture—so visible in any honest Alexander Fleming biography—is what turns an anecdote into a method.
What the Discovery Changed in Everyday Medicine
Before antibiotics, a scratch from a rose bush could become a funeral. Childbirth could turn septic in hours. Pneumonia stalked the winter. With penicillin and its successors, appendectomies became routine rather than lethal gambles; orthopedic surgery could implant foreign materials; dentists could manage abscesses with confidence; and case-fatality rates for bacterial pneumonias and septicemias plummeted. The shift was not only clinical but psychological: infection moved from inevitability to challenge, a through-line in any serious Alexander Fleming biography.
Reputation, Recognition, and the Perils of Fame
Fleming accepted honors with deflationary humor. Fame magnifies stories and simplifies heroes. For a time he became a polite celebrity—asked to give talks, pose for photographs, and offer a kind of secular benediction on medical progress. That visibility helped public support but risked nuance. He worked to keep the narrative factual: he praised the Oxford team, described his own limits, and kept demonstrating plates that persuaded. The Alexander Fleming biography is thus also a map of responsible credit.
Teaching With Fleming: Lessons for Students and Makers
If you teach a methods course, his story is a near-perfect scaffold. Ask students to design a plate that would make a halo visible. Have them write a one-page “failure report” for an unstable extract. Assign his early lysozyme notes and later penicillin work; compare what stayed constant in his thinking. Even outside biomedicine, teams can adopt the stance at the heart of the Alexander Fleming biography: prepare the stage, then let the world surprise you.
The Global Arc: From London to Everywhere
A generation after penicillin, antibiotics threaded themselves into the global economy—from Peoria’s tanks to post-war Japanese fermentation labs, from British hospitals to South American clinics. International agencies track resistance; national formularies debate access and price; agricultural policies wrestle with veterinary stewardship. The Alexander Fleming biography now unfolds on a planetary stage where logistics, equity, and evolution meet.
Lysozyme: The Prequel That Explained the Sequel
Histories that rush to penicillin skip an invention of nature Fleming brought into focus earlier: lysozyme. The enzyme would not become a blockbuster therapy, but it trained a generation of eyes to look for antimicrobial clues in ordinary physiology—tears, saliva, mucus. Mechanistically, lysozyme nicks bonds in the bacterial cell wall, weakening the lattice that maintains shape and pressure. In the lab, colonies that once looked crisp soften, like chalk turning to damp powder. The delight Fleming took in that ordinary magic says much about the Alexander Fleming biography: start with the humble, then make it precise.
The 1929 Paper and the “Crude Extract” Years
Fleming’s first formal description of penicillin’s action (1929) reads today as a model of clarity and restraint: zones of inhibition that speak for themselves, lists of organisms tested, and notes about fragility. Visitors sometimes left St Mary’s with small quantities of penicillin-containing filtrates—brownish, unstable, impure. Superficial infections sometimes responded; deeper infections did not. Without purification, the active principle could not reach therapeutic levels. The frustration is a key chapter in any Alexander Fleming biography: promise outran tools until chemistry, engineering, and clinical trial craft caught up.
Oxford, Peoria, and the Art of Scaling Up
When Florey and Chain revived the program, they did so with a modern architecture: biochemists shoulder-to-shoulder with clinicians; animal facilities next to chemistry benches; statisticians close enough to be annoying and indispensable. In mice with otherwise fatal infections, purified fractions reversed the course of disease. Early clinical cases mixed triumph and heartbreak—a policeman improved dramatically until the stock ran out, then died—galvanizing efforts to scale. Deep-tank fermentation, air-sparging, and corn-steep liquor turned scarcity into supply; “Moldy Mary” Hunt’s cantaloupe strain became a folk hero of process science.
Public Health, Surgery, and the New Baseline of Risk
Modern medicine’s confidence rests on antimicrobial backstops. The safety of cesarean sections, the viability of joint replacements, the ease with which dentists drain abscesses, the success of oncology regimens—all presume credible antibiotics nearby. The Alexander Fleming biography thus underwrites much of contemporary care: new sterility routines in operating theaters, susceptibility testing in labs, formularies in pharmacies, and discharge instructions that teach patients how to finish courses responsibly.
Resistance Wasn’t a Surprise—It Was the Premise
If a substance can kill, evolution can select for a microbe that dodges or degrades it. Early lab work showed that sub-lethal exposures can yield survivors with thicker walls, altered targets, or enzymes that blunt the drug’s edge. Medicine responded with beta-lactams that resist bacterial enzymes, combination therapies that pair a drug with an inhibitor, and prescribing rules that favor precise diagnoses over reflexes. The Alexander Fleming biography anticipated this arc: celebrate potency, but plan for its erosion.
Communicating Science Without Simplifying It Away
Fleming’s plain voice made him durable. He did not use discovery to claim omniscience; he used it to warn and persuade. When the spotlight found him, he reflected some of it onto colleagues and onto the institutions that turned an observation into a medicine. Big advances tempt hero narratives; the better story insists on networks and on unglamorous, careful work at the right times. That ethic threads the Alexander Fleming biography from bench to podium.
Places of Memory: Museums, Labs, and the Stories We Tell
Medical museums often stage a 1920s lab: wooden benches, glass desiccators, a microscope, trays of plates. The spectacle is pedagogy, not nostalgia. Seeing the modesty of the tools refreshes respect for craft. At St Mary’s, exhibits preserve the feel of rooms where plates were poured and where a returning scientist noticed a clear circle. Archives display notebooks and photographs, patient case notes and supply requisitions—reminding us that the “miracle” was many small procedures done well.
What Clinicians Still Learn From the Story
Beyond inspiration, penicillin’s story leaves practical maxims. Take samples before the first dose—labs cannot culture what they never see. Use the narrowest effective agent—broad spectrum pressures bystanders you did not intend to target. Consider the site of infection—cell-wall agents behave differently in cerebrospinal fluid than in bone. Attend to host factors—history of allergy, renal function, immune status. Plan the stop date when you plan the start. Document, teach, and improve—habits that echo throughout any serious Alexander Fleming biography.
Why These Lines Still Circulate
Short lines survive because they carry layered advice. “Nature did that” is humility and method at once: look first to the world for mechanisms to adopt and adapt. “It does not teach” is a plea to protect judgment from the flattering illusion that a strong drug absolves bad practice. The reminders are evergreen because the temptations—overconfidence, shortcuts, one-size-fits-all fixes—are evergreen.
Closing Reflections: A Biography That Doubles as a Map
The most responsible way to tell this story is to let it remain complicated. The Alexander Fleming biography should not be reduced to a parable about lone genius or to a sermon about luck. It is a map of how science works when it matters: observation sharpened by craft, enriched by collaboration, validated by careful trials, scaled by engineers, stewarded by public health, and argued about by ethicists and economists. That is how a small clear circle on a plate became a durable civic good.