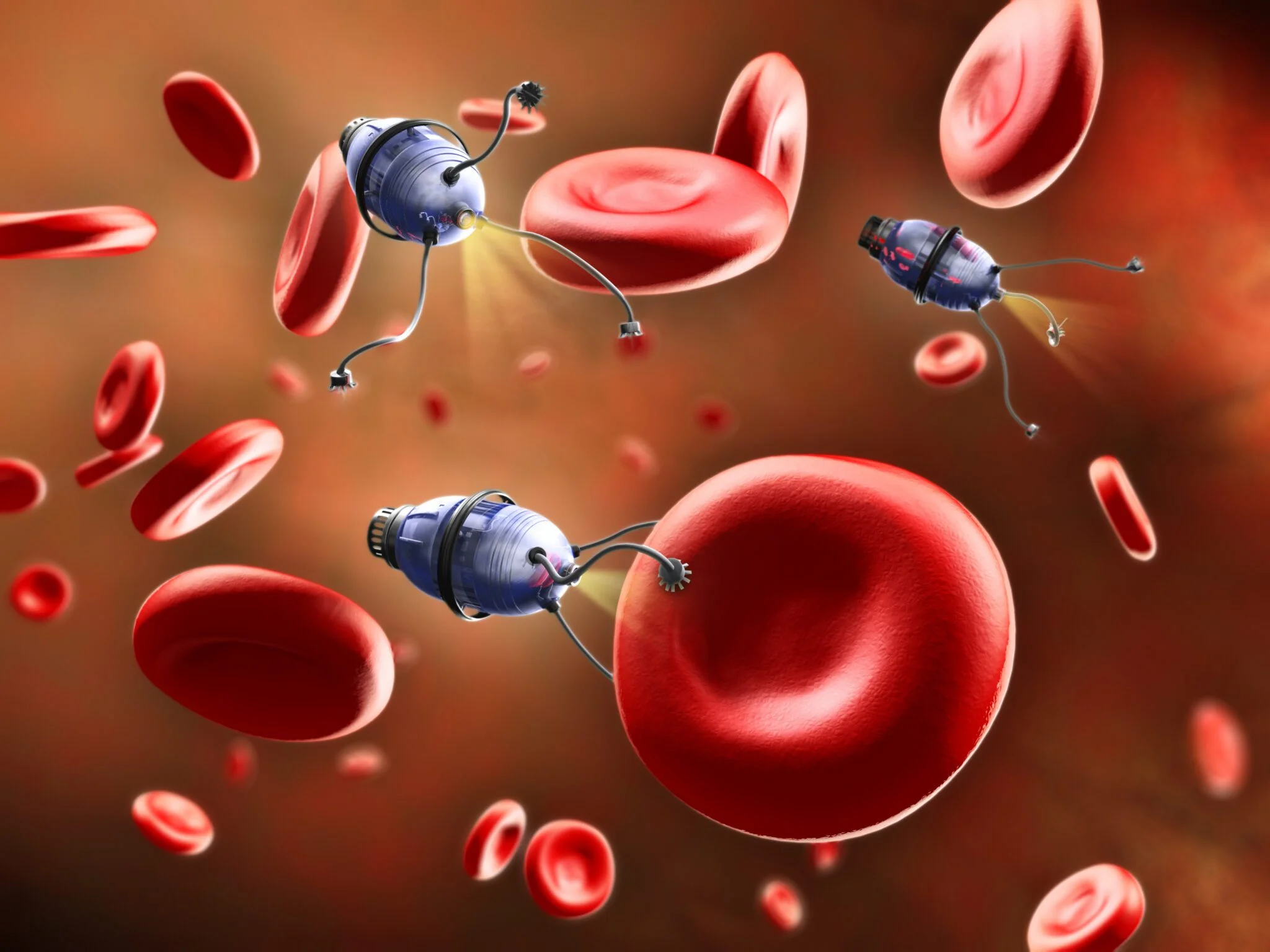
In the fight against cancer, a powerful new ally has emerged—nanomedicine cancer therapy. Unlike traditional methods that often cause collateral damage to healthy tissues, this emerging discipline offers a precise, personalized approach to targeting cancer cells. Using nano-sized particles engineered to navigate the body with pinpoint accuracy, scientists are rewriting the rules of cancer treatment. In this article, we’ll explore the science behind nanomedicine, its current applications in oncology, and how it’s paving the way for safer, more effective therapies.
The Science Behind Nanomedicine
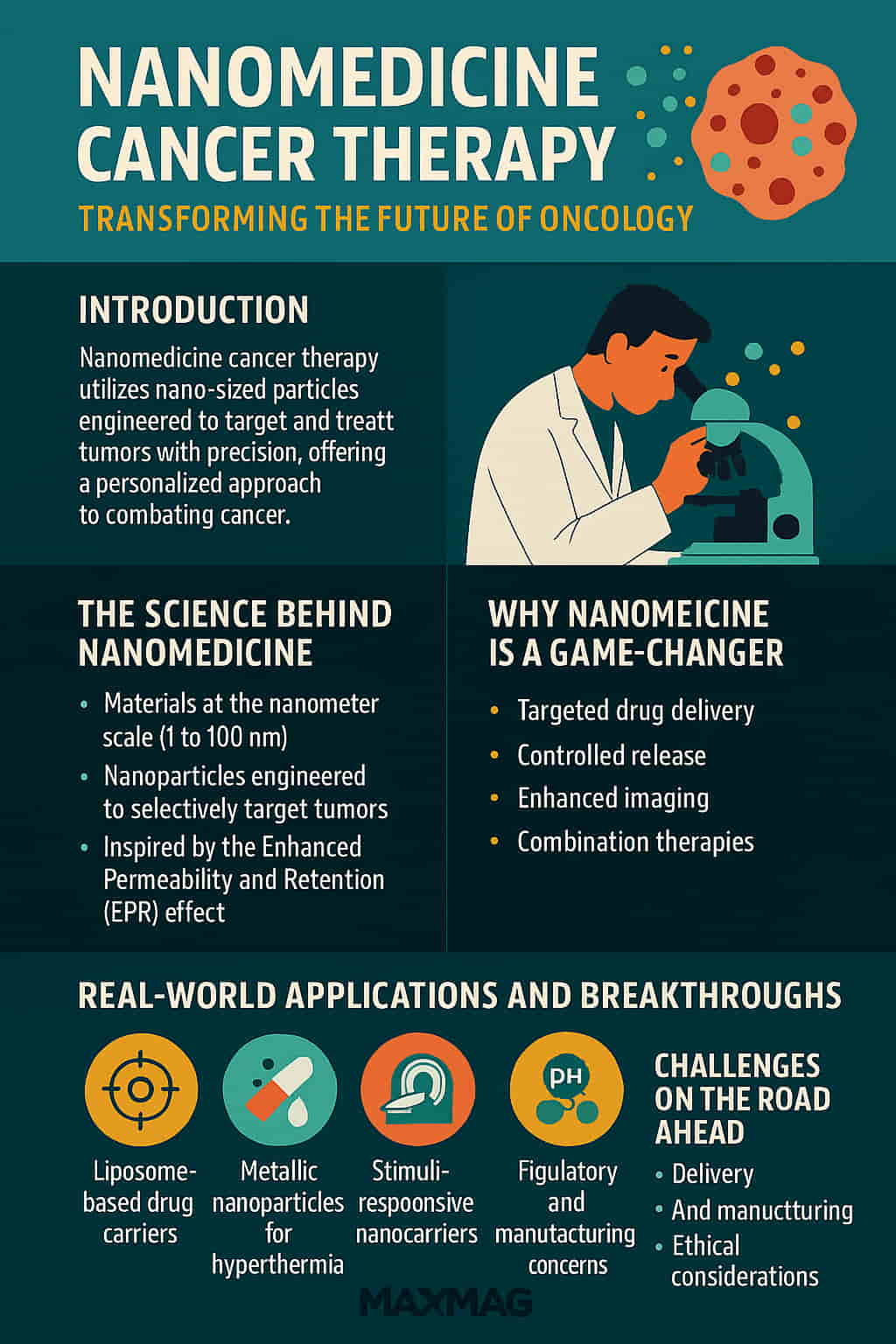
At its core, nanomedicine involves the use of materials at the nanometer scale—typically between 1 and 100 nanometers—to diagnose, monitor, and treat diseases. When applied to cancer, the goal is to develop nanoparticles that can selectively target tumors while minimizing exposure to healthy cells.
Cancerous tumors often have leaky blood vessels, a phenomenon known as the Enhanced Permeability and Retention (EPR) effect. This makes them particularly susceptible to the accumulation of nanoparticles, which can be loaded with chemotherapy drugs, imaging agents, or heat-generating materials.
For example, a nanoparticle might be designed to remain inert while circulating in the bloodstream but activate and release its drug payload only when it reaches the acidic environment of a tumor. This kind of “smart delivery system” is at the heart of nanomedicine cancer therapy.
Why Nanomedicine Is a Game-Changer in Cancer Treatment
Traditional chemotherapy and radiation therapy can be effective, but they often come at a steep cost to the patient’s overall health. These treatments are notorious for damaging fast-growing healthy cells, which leads to side effects like hair loss, nausea, fatigue, and compromised immune function.
By contrast, nanomedicine cancer therapy offers several key advantages:
-
Targeted drug delivery: Medications reach the tumor more directly, reducing toxicity.
-
Controlled release: Drugs can be designed to release slowly or in response to specific conditions.
-
Enhanced imaging: Nanoparticles can be used as contrast agents to improve MRI and CT scans.
-
Combination therapies: Nanoparticles can carry multiple agents—such as a drug and a heating compound—enabling synchronized attacks on cancer cells.
In short, nanomedicine doesn’t just aim to destroy cancer—it seeks to do so with intelligence and precision.
Real-World Applications and Breakthroughs
The idea of treating cancer with nanoparticles might sound like science fiction, but it’s already moving from the lab to the clinic. Some of the most promising applications include:
1. Liposome-Based Drug Carriers
One of the earliest and most successful applications of nanomedicine has been the development of liposomal drug carriers. These tiny spherical vesicles can encapsulate chemotherapy drugs like doxorubicin and deliver them more efficiently to tumor cells.
Doxil, the first FDA-approved liposomal form of doxorubicin, has shown improved outcomes in treating ovarian and breast cancer, with fewer side effects compared to traditional administration.
2. Metallic Nanoparticles for Hyperthermia
Gold and iron oxide nanoparticles are being studied for their ability to generate heat when exposed to specific types of light or magnetic fields. When these particles accumulate in tumors, they can be activated to raise the local temperature, effectively “cooking” the cancer cells while leaving nearby tissues unharmed.
Research from the National Cancer Institute shows that magnetic hyperthermia may improve treatment outcomes when combined with chemotherapy, especially for deep-seated tumors like those in the pancreas or brain. Source: cancer.gov
3. Stimuli-Responsive Nanocarriers
Some nanoparticles are designed to respond to internal biological cues such as enzymes, pH changes, or redox states. These “smart” systems ensure that drugs are only released when they encounter the unique environment of a tumor.
Such precision not only boosts efficacy but also reduces drug resistance—a growing problem in conventional cancer therapy.
Challenges on the Road Ahead
Despite its enormous promise, nanomedicine cancer therapy is not without challenges. Many of the technologies are still in experimental stages and face hurdles before they can be widely adopted.
Delivery and Targeting
Ensuring that nanoparticles reach the tumor and stay there long enough to be effective is a significant challenge. The body’s immune system may recognize these particles as foreign and eliminate them before they reach their target.
To overcome this, scientists are developing “stealth” nanoparticles coated with substances like polyethylene glycol (PEG) to evade immune detection.
Regulatory and Manufacturing Concerns
Because nanomedicine represents a new frontier, regulatory pathways are still evolving. Ensuring quality control, safety, and efficacy at scale requires rigorous testing and significant investment.
Moreover, manufacturing nanoparticles consistently and affordably remains a bottleneck. Small changes in size or composition can drastically alter how a particle behaves in the body.
Nanomedicine Cancer Therapy and Personalized Medicine
One of the most exciting aspects of nanomedicine cancer therapy is its potential to enable truly personalized medicine. By analyzing a patient’s unique tumor profile, doctors can design nanoparticles tailored to specific molecular targets. This customized approach not only increases the likelihood of success but also minimizes side effects.
For instance, nanoparticles can be equipped with antibodies that recognize specific markers on cancer cells. Once the particle binds to the target cell, it can release its therapeutic cargo directly into the cell’s interior. This level of precision holds promise for treating even the most resistant forms of cancer.
Ethical Considerations
With new technology comes new responsibility. Nanomedicine raises several ethical questions, particularly around safety, privacy, and access.
-
Safety: Long-term effects of nanoparticles are not fully understood. Could they accumulate in organs over time?
-
Privacy: Smart nanoparticles that transmit data about a patient’s condition raise concerns about data security.
-
Access: Will these cutting-edge treatments be available only to wealthy patients or to all who need them?
Addressing these concerns will be critical as nanomedicine moves toward mainstream adoption.
The Future of Cancer Therapy Is Nano
As technology advances, we can expect nanomedicine cancer therapy to become more refined, more personalized, and more powerful. New types of nanoparticles are being developed that can deliver multiple drugs, act as imaging tools, and even report back on the tumor’s response to treatment.
Moreover, integrating nanomedicine with artificial intelligence could open new doors for real-time monitoring and adaptive treatment strategies. AI can analyze massive datasets to predict how a patient will respond to a particular nanoparticle, allowing doctors to adjust treatments dynamically.
Trusted Resources for Further Reading
For readers interested in digging deeper into the science of nanomedicine and its clinical applications, the following U.S.-based resources provide reliable, up-to-date information:
These sites are excellent starting points for both patients and professionals seeking to understand the evolving landscape of cancer treatment.
Frequently Asked Questions (FAQ)
Q1: What is nanomedicine cancer therapy?
A: It’s a form of cancer treatment that uses nano-scale materials to deliver drugs, heat, or other therapeutic agents directly to tumor cells.
Q2: Is nanomedicine already being used in hospitals?
A: Yes, certain nanomedicine-based drugs like liposomal chemotherapy agents are FDA-approved and used in clinical settings.
Q3: What are the benefits over traditional treatments?
A: Nanomedicine offers targeted delivery, fewer side effects, and the potential for personalized treatment based on a patient’s biology.
Q4: Are there risks involved?
A: While generally considered safe, long-term studies are still needed to fully understand how nanoparticles interact with the human body over time.
Q5: Will nanomedicine replace chemotherapy and radiation?
A: Rather than replacing them entirely, nanomedicine is expected to enhance these treatments by making them more effective and less toxic.