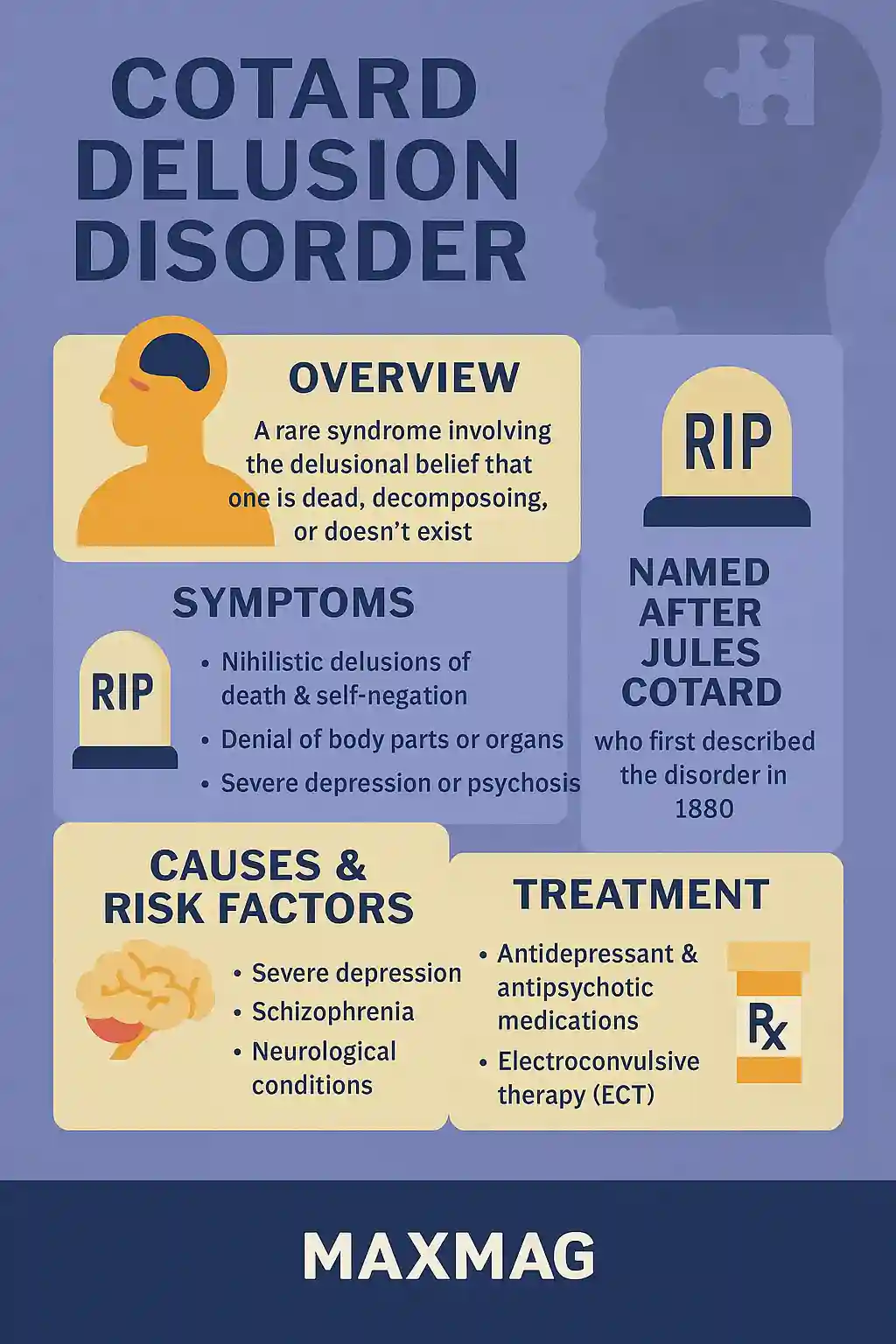
At first glance, it sounds like fiction: a person convinced they are dead, decomposing, or entirely non-existent. Yet this rare and haunting psychiatric condition is a real and medically documented phenomenon known as Cotard’s syndrome. Named after French neurologist Jules Cotard, this delusion grips individuals with the unsettling belief that they’ve lost their organs, blood, soul—or even that they no longer exist altogether.
What makes this disorder so chilling isn’t just the surreal nature of its symptoms, but how deeply it reflects the complexities of human consciousness and identity. Exploring Cotard delusion disorder offers a window into the fragile wiring of perception, self-awareness, and brain function.
What Is Cotard Delusion?
Cotard’s syndrome, often referred to as “walking corpse syndrome,” is a type of nihilistic delusion, a severe mental state in which the person genuinely believes they are dead or no longer exist. While rare, it has been identified across many cultures and age groups, though it most often affects individuals with underlying mental health disorders such as severe depression, schizophrenia, or neurological damage.
In clinical terms, Cotard delusion disorder is not a standalone diagnosis but a symptom complex usually arising in the context of major psychiatric illness. What’s notable is the unwavering conviction of the belief—no matter how irrational it may seem to others.
The First Known Case and Historical Background
The disorder was first formally documented in 1880 by Jules Cotard, who described a female patient convinced she had “no brain, nerves, chest, or entrails.” She insisted she didn’t need to eat because she was already dead. This early case established the foundation for what is now known as the Cotard delusion disorder, and it has remained a fascinating clinical mystery ever since.
Modern psychiatry has since identified a range of cases, including people who refuse food or hygiene because they believe such acts are pointless if one is dead. In some instances, sufferers even visit morgues or request death certificates.
Brain Dysfunction and Neurological Roots
Neuroscientific studies have revealed that Cotard’s syndrome often involves dysfunction in brain regions responsible for facial recognition and emotional processing. Specifically, researchers have pointed to the fusiform gyrus (which processes facial identity) and the amygdala (which governs emotional response) as key players. When these systems are disconnected or impaired, a person might recognize themselves or others visually but feel emotionally detached—leading to delusions that their body or identity has ceased to exist.
This phenomenon bears similarity to Capgras syndrome, another rare condition in which individuals believe loved ones have been replaced by impostors. Both reflect distorted perceptions of self and others, likely rooted in neurobiological disconnection.
According to experts at the National Institute of Mental Health, brain-based disruptions in mood and perception—especially in cases involving depression with psychotic features—can significantly heighten vulnerability to Cotard-like symptoms.
Risk Factors and Comorbid Conditions
Cotard delusion disorder is rarely seen in isolation. It typically appears alongside:
-
Major depressive disorder
-
Psychotic disorders, including schizophrenia
-
Bipolar disorder, particularly during depressive episodes
-
Dementia or Alzheimer’s disease
-
Neurological conditions, including traumatic brain injury and stroke
In some rare instances, it’s also been linked to substance withdrawal or medical conditions such as tumors or epilepsy.
Importantly, many of these comorbidities are characterized by disruptions in self-concept, perception, and emotional regulation—all fundamental elements implicated in Cotard’s.
The Emotional and Social Toll
Imagine the terror of believing you’re no longer alive—unable to feel, connect, or belong. For those experiencing Cotard’s, life can feel like a surreal prison. Many sufferers isolate themselves, stop eating or drinking, and engage in dangerous behavior due to their delusions.
Studies highlighted by Harvard Medical School show that untreated Cotard syndrome can lead to self-neglect, suicidal ideation, and even fatal outcomes if patients refuse medical care. This underlines the urgency of early detection and treatment.
Diagnosis: A Psychiatric Puzzle
There is no definitive test for Cotard syndrome. Diagnosis typically involves a detailed psychiatric assessment and ruling out neurological causes through imaging (such as MRIs or CT scans). Clinicians look for signs of nihilistic delusions, alongside other mood or psychotic features.
Given its rarity, Cotard’s syndrome can sometimes be misdiagnosed as major depression, schizophrenia, or even dementia—especially in older adults. This makes comprehensive evaluation crucial to tailor effective treatment.
Treatment: From Antidepressants to ECT
Fortunately, Cotard’s syndrome is treatable in many cases. Management typically includes a combination of:
-
Antidepressants, particularly SSRIs or SNRIs
-
Antipsychotic medications for delusional features
-
Mood stabilizers in bipolar-related cases
-
Electroconvulsive therapy (ECT)—one of the most effective treatments, especially when pharmacological solutions fail
In fact, ECT has been remarkably successful in reversing Cotard delusion disorder, especially in cases linked to severe depression. It helps recalibrate neural activity patterns, lifting the fog of nihilism in many patients.
Psychotherapy, especially cognitive behavioral therapy (CBT), may also play a role, although it is most effective once the delusion has begun to subside pharmacologically.
Real Case Example
One widely reported case involved a 53-year-old woman who, following a head injury, developed the firm belief she had died and was in hell. She asked to be taken to a morgue and refused food. With treatment involving both antipsychotics and ECT, her delusion gradually lifted—and she fully regained her sense of self.
This is just one of many harrowing but ultimately hopeful stories that demonstrate that Cotard delusion disorder can be overcome with timely and appropriate intervention.
Cotard’s Syndrome and Pop Culture
Cotard’s syndrome has made brief appearances in pop culture, often inaccurately. Films, books, and TV shows sometimes sensationalize the idea of someone believing they’re dead, but these depictions rarely capture the true despair and complexity of the condition.
Nonetheless, public awareness—even when imperfect—can spark curiosity and reduce stigma, encouraging those affected to seek help.
A Mirror of the Mind’s Fragility
Ultimately, Cotard’s syndrome forces us to confront the delicate boundary between body, mind, and identity. The disorder serves as a stark reminder of how much brain chemistry influences our sense of reality—and how easily that perception can fracture.
To better understand emotional development in children and the importance of psychological support from a young age, see this related article on fairy tales and child psychology, which explores how imagination shapes self-concept and emotional regulation—tools that help protect against delusional breakdowns later in life.
❓ FAQ: Cotard Delusion Disorder
Q1: Is Cotard’s syndrome curable?
A: While rare and severe, it is often treatable, especially when caught early. Many patients recover fully with proper psychiatric and medical support.
Q2: How common is Cotard delusion disorder?
A: Extremely rare. Fewer than a few hundred documented cases exist globally.
Q3: Is it dangerous?
A: Yes. The belief of being dead can lead to self-neglect, starvation, or self-harm, making treatment essential.
Q4: Can it happen without mental illness?
A: It’s rare but possible, especially following traumatic brain injuries or severe stress. Most cases, however, are tied to major psychiatric conditions.
Q5: What’s the most effective treatment?
A: Electroconvulsive therapy (ECT) has shown significant success, particularly in cases stemming from major depression.